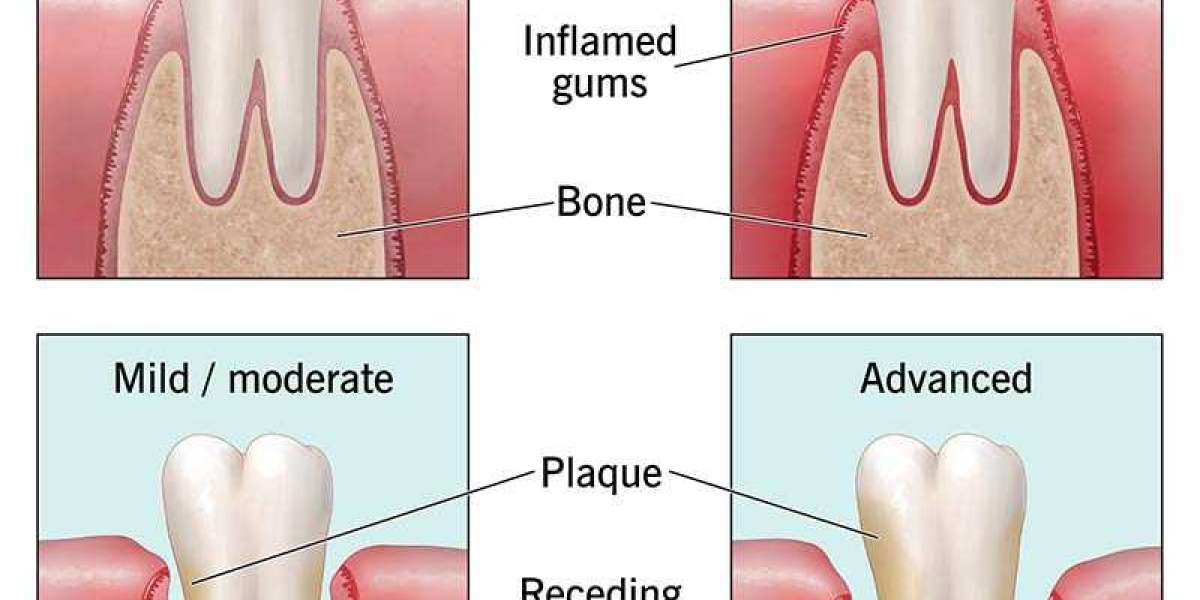
Periodontitis is a chronic inflammatory disease that affects the gums, periodontal ligament, and supporting bone around the teeth. It is one of the leading causes of tooth loss in adults worldwide and has been linked to broader systemic issues such as cardiovascular disease, diabetes, and inflammatory disorders.
While oral hygiene practices like brushing, flossing, and regular dental visits remain essential for preventing periodontal disease, emerging research increasingly highlights the profound influence of nutrition on gum health.
A nutrient-rich diet not only strengthens the immune system but also reduces inflammation, enhances tissue repair, and supports the oral microbiome all of which are essential in preventing the onset and progression of periodontitis.
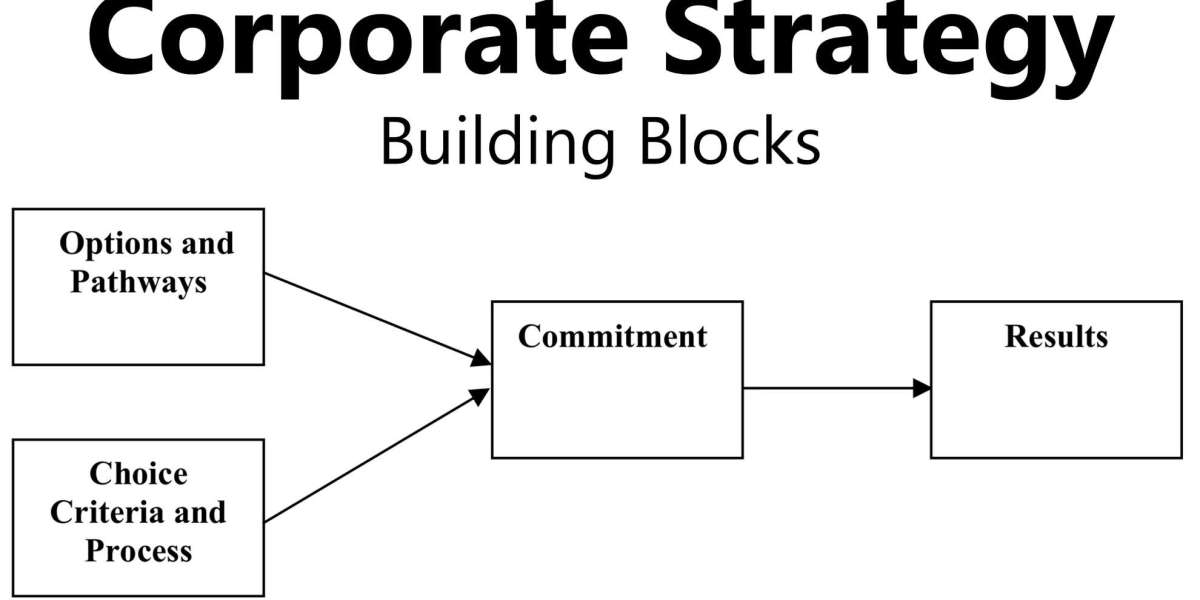
Interestingly, discussions around health products from oral health supplements to pharmaceuticals often appear alongside commercial topics such as supply chains and procurement. For example, industries involved in sourcing dental-care products may operate similarly to how a mebendazole wholesaler distributes antiparasitic medications.
Although unrelated in purpose, both illustrate how health-related needs rely on accessible, high-quality products. In the case of periodontal disease, however, nutrition remains one of the most accessible preventive tools for the general public.
Understanding the Link Between Nutrition and Periodontal Disease
Periodontitis begins with plaque accumulation, but its progression into a destructive inflammatory condition depends heavily on the host's immune response. Nutritional factors influence:
immune system efficiency,
inflammatory pathways,
antioxidant capacity,
tissue regeneration, and
oral microbial balance.
Deficiencies in key nutrients weaken the body’s ability to fight harmful bacteria and repair damaged gum tissues. Conversely, a nutrient-rich diet strengthens periodontal resilience.
Key Nutrients That Support Gum Health
1. Vitamin C
Vitamin C is among the most studied nutrients regarding gum health. It plays a central role in collagen synthesis, which is essential for maintaining the structural integrity of gingival tissues. A deficiency can cause swollen, bleeding gums one of the early signs of periodontal disease.
Sources include:
citrus fruits (oranges, lemons),
berries,
peppers,
leafy greens like spinach and kale.
Adequate vitamin C intake reduces inflammation and supports healing, making it a cornerstone nutrient for periodontal health.
2. Vitamin D
Vitamin D helps regulate immune responses and supports bone density. Since periodontitis involves bone deterioration around teeth, maintaining appropriate vitamin D levels is crucial. Low vitamin D levels have been directly associated with increased periodontal pockets and attachment loss.
Sources include:
sunlight exposure,
fortified dairy products,
fatty fish (salmon, sardines).
Vitamin D also aids calcium absorption, contributing to stronger teeth and jawbone structure.
3. Calcium
Calcium is essential for building and maintaining alveolar bone the bone that supports teeth. Research shows that individuals with low calcium intake are more likely to experience tooth mobility and bone loss.
Calcium-rich foods include:
dairy products,
almonds,
tofu,
leafy greens.
Combined with vitamin D, calcium ensures structural stability in the mouth.
4. Omega-3 Fatty Acids
Omega-3s are powerful anti-inflammatory agents. They can reduce periodontal inflammation by inhibiting cytokines that trigger tissue destruction. Studies have shown that diets rich in omega-3 fatty acids are associated with improved periodontal outcomes and reduced disease severity.
Sources include:
salmon,
flaxseeds,
walnuts,
chia seeds.
Omega-3 supplementation has even been explored as a complementary periodontal therapy.
5. Antioxidants
Antioxidants combat oxidative stress, which plays a significant role in periodontal disease progression. Vitamins A and E, selenium, and polyphenols help neutralize free radicals, thus reducing tissue damage.
High-antioxidant foods include:
green tea,
berries,
nuts and seeds,
colorful vegetables.
Green tea, in particular, contains catechins that exhibit strong antibacterial and anti-inflammatory effects.
6. Probiotics
The oral microbiome is a crucial factor in periodontal health. Probiotics, especially strains like Lactobacillus reuteri, help balance harmful and beneficial bacteria, reducing the risk of inflammation and periodontal breakdown.
Probiotic sources include:
yogurt and kefir,
fermented vegetables like kimchi and sauerkraut,
probiotic supplements.
Probiotic therapy is increasingly recognized as a promising adjunct to periodontal treatment.
Foods That Promote or Prevent Inflammation
Diet plays a direct role in inflammation, which is central to periodontitis. Consuming excessive processed foods high in sugar, refined grains, and unhealthy fats promotes systemic inflammation. These foods also create an acidic oral environment that fosters harmful bacterial growth.
Particularly harmful dietary patterns include:
high sugar intake (fuels plaque bacteria),
frequent snacking (reduces protective saliva),
processed meats (linked to inflammation),
refined carbohydrates (increase glycemic load).
In contrast, anti-inflammatory diets such as the Mediterranean diet rich in fruits, vegetables, whole grains, olive oil, nuts, and lean proteins are associated with reduced periodontal inflammation and better clinical outcomes.
Hydration and Saliva Production
Saliva plays a protective role in oral health by neutralizing acids, washing away food particles, and delivering essential minerals to teeth. Poor hydration can reduce saliva flow, increasing susceptibility to gum irritation and bacterial overgrowth.
Drinking adequate water also supports overall metabolic health, which indirectly contributes to stronger periodontal defenses.
Sugar: The Critical Risk Factor
Sugar fuels the growth of pathogenic bacteria such as Porphyromonas gingivalis, a major contributor to periodontitis. Additionally, high sugar intake spikes blood glucose levels, impairing immunity and slowing healing particularly in individuals with diabetes, who are already at higher risk for gum disease.
Reducing added sugar intake is one of the most effective dietary strategies for preventing both cavities and periodontal disease.
Nutrition and Systemic Health: A Dual Impact on Periodontitis
Periodontal disease is not limited to the mouth; it is connected to systemic conditions like diabetes, metabolic syndrome, and cardiovascular disease. Poor nutrition increases the risk for these conditions, creating a cycle of inflammation that also worsens gum health. A nutritious diet helps break this cycle by stabilizing blood sugar, reducing systemic inflammation, and supporting immune efficiency.
Practical Dietary Recommendations for Preventing Periodontitis
Consume a variety of colorful fruits and vegetables daily to ensure adequate antioxidants.
Increase intake of omega-3-rich foods such as nuts and fatty fish.
Choose whole grains over refined carbohydrates.
Limit sugary snacks and beverages, replacing them with water or unsweetened alternatives.
Ensure adequate calcium and vitamin D intake, especially for older adults.
Include probiotic foods to support a balanced oral microbiome.
Stay well-hydrated to support saliva production.
Conclusion
Nutrition plays a fundamental role in preventing and managing periodontitis. While brushing, flossing, and professional cleanings remain essential, the foods we consume directly influence inflammation, immune response, bone health, and the oral microbiome. A balanced, nutrient-rich diet supports strong gums and teeth while reducing the risk of chronic oral disease.
Just as reliable access to quality products whether through a mebendazole wholesaler or a dental supply distributor contributes to overall public health, consistent access to nutritious foods is equally essential. By prioritizing whole, nutrient-dense foods and minimizing inflammatory dietary habits, individuals can significantly reduce their risk of periodontal disease and promote lifelong oral health.